COVID-19 - A Complete Overview
Table of Contents
- Introduction
- Overview - Science Basics
- Lockdown Viewpoints
- How the UK Government handled the pandemic
- The Impact of COVID-19 on Patients
- General impact on patients
- Patients with chronic disease
- Patients over 60 & Care Homes
- Patients in BAME communities
- Conclusion
Introduction
Hot topics questions are a common theme in medical school interviews. It is important as an aspiring medical student that you are able demonstrate your interest and understanding of key issues affecting healthcare and the NHS.
Within the last year COVID-19 has had a significant impact on the world with regards to health, economics, ethics and politics. There is a lot of information out there about COVID-19: the information is dense, and is changing very quickly. In this post we hope to give you a general overview of the key aspects of COVID-19 in terms of the science and the impact the virus has had on the public, NHS and the government. It is essential that you have a clear grasp of these elements so that you can confidently discuss them at interview and are able to consider the impact of COVID-19 from different perspectives.
Read more about COVID-19 basics here

Overview - Science Basics
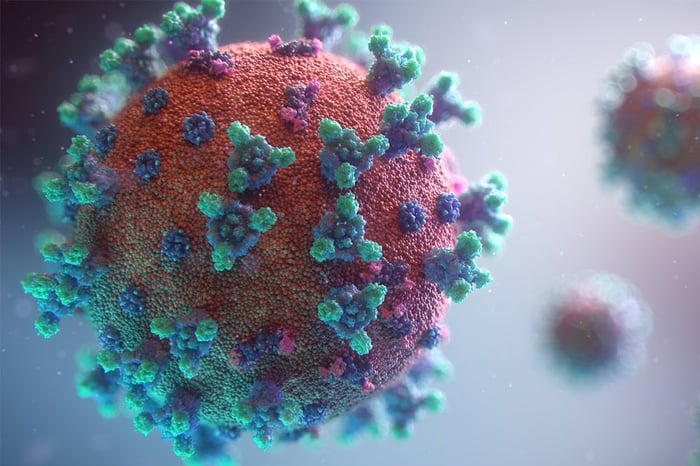
COVID-19 is an infectious disease that belongs to the Coronavirus family. Coronaviruses cause respiratory infections in humans and animals which can range from mild colds to deadly disease. Coronaviruses cause about one-quarter of all common colds. However some strains of the virus can be far more dangerous and spread rapidly. In 2020 COVID-19 caused a global pandemic with a rapidly rising number of cases spanning across the world.
COVID-19 is spread through liquid particles produced by an infected person. Small liquid particles are present in an infected person’s mouth or nose and dispersed in the air when they cough, speak or sneeze. These droplets can then transmit into another person’s mouth or nose, when people are close to each other or from touching a contaminated surface. Some smaller droplets can also remain in the air and cause airborne transmission. This knowledge has led to widespread worldwide recommendations such as social distancing, regular hand washing and wearing a mask to prevent transmission.
Once exposed to the virus there is an incubation period before the appearance of first symptoms. According to the WHO this can range from 1-14 days. The three main symptoms of COVID-19 are: high temperature, new continuous cough, or a loss or change in sense of smell or taste, however many people can be asymptomatic. As the symptoms of COVID-19 are non-specific, those who have been exposed are advised to self isolate even if they have no symptoms. Early recognition and testing is key to preventing transmission.
Currently there is no cure for COVID-19. Around 80% of patients recover without any medical input, however those with a more severe presentation may require supportive treatment such as oxygen therapy, fluids, and ventilation. Some of the complications of COVID-19 include respiratory or lung failure, blood clots, heart attacks, and tragically death in the worst cases. Clinical trials remain underway to find more robust treatment options but the main strategies to control the virus have been social distancing measures, lockdowns and the development of a vaccine programme.

Lockdown Viewpoints
The COVID-19 pandemic has been a uniquely challenging situation for governments around the world. There are curfews, quarantines, and other restrictions in place in many countries with the hope of reducing the spread of the virus. With nearly 4 billion people facing some form of lockdown in more than 90 countries, there is bound to be disagreement about the best way through this pandemic.
Pro-Lockdown
Arguments in favour of prioritizing restrictive measures are the high transmission and mortality rate of COVID-19. According to the European Centre for Disease Prevention and Control, one person infected with COVID-19 will on average infect between two and three other people. The mortality rate of COVID-19 is higher than that of other common contagious diseases such as seasonal flu. The World Health Organization estimates that the global crude mortality rate is between 3-4%. COVID-19 is more likely to cause serious illness or death in people over 60 years old as well as people with underlying medical problems such as high blood pressure, heart/lung disease, diabetes, obesity, and cancer. Prioritizing the safety of these vulnerable groups is the morally correct thing to do.
The burden on health services must also be considered. At the beginning of the COVID-19 pandemic, there was a fear that hospital admissions for COVID-19 would outstrip hospital capacity, resulting in deaths that would otherwise have been preventable. There is also a limited number of intensive care beds. It is vital that we do not have more people that need ICU than hospitals can accommodate.
There is currently no cure for COVID-19. The vaccine programme is underway however it will take many months to effectively vaccinate the population. Therefore, it can be argued that we must use non-pharmacological options to stop the virus from spreading. This includes strategies such as physical distancing, hygiene, masks, isolation of infected people and their contacts, and lockdowns, such as closures of school and businesses and bans on public gatherings and travel.
Read more about this topic in detail
Anti-Lockdown
Many have argued that lockdowns infringe on the democratic values of freedom and civil rights. Although the aim of lockdown is to protect people, it has potentially harmful consequences on society. During the first lockdown in the United Kingdom thousands of cases of cancer went untreated, two-thirds of adults with mental health problems reported a worsening of their condition and the number of suicide and attempted suicide incidents surged up 68% from the previous year. Damage to the economy must also be considered; the UK is in the largest recession on record.
In the UK there has also been huge disruption to the education system due to school closures. The Human Rights Act states that “no person shall be denied the right to education” and that “everyone has the right to respect for his private and family life, his home and his correspondence”. Therefore, we must think carefully about the impact of restrictions.
Research has demonstrated that lockdowns are not a long-term solution. The main issue is that immunity to coronaviruses does not last long and reinfection is possible. Therefore, “herd immunity” is not possible to achieve with lockdown measures alone. Other less restrictive measures which have been suggested include increased testing and tracing, isolating people and creating small social bubbles.
There have been several anti-lockdown protests in the UK in relation to the COVID-19 pandemic. They argue is it fair to impose radical limits on the freedom of all with no apparent end in sight? Although thousands of lives are being saved millions of young people are seeing their prospects sacrificed.
Read more about this topic in detail

How the UK Government handled the pandemic
The COVID-19 pandemic has been one of the biggest peace-time challenges facing the UK government. As of the 6th January 2021, the UK has had over 2.7 million people test positive for COVID-19 and over 80,000 deaths. The UK government has taken many measures to try to control the COVID-19 pandemic. Interviewers will often ask for your opinion on the handling of the pandemic so it is important that you can grasp the UK government’s response from various perspectives.
The UK government introduced a series of laws to stop people spreading the virus by implementing lockdowns. The UK government introduced its first national lockdown at the end of March 2020 which lasted for around 7 weeks. There was another month-long national lockdown in November 2020 and a third national lockdown started in January 2021. In addition to this, there have been a series of local measures introduced throughout the pandemic.
Many businesses have been forced to stop operating due to COVID-19 restrictions. In order to help these struggling businesses to survive the UK government has provided substantial financial support such as grants, loans and devised a job retention scheme.
The UK government faced a huge challenge in making sure that the National Health Service could cope with the pandemic. The NHS received £6.6 billion from the UK government’s coronavirus emergency fund. There were also the enormous tasks of supplying personal protective equipment (PPE) to health and social care workers, as well as increasing the testing capacity for COVID-19. Additional funding was directed towards research into treatments and vaccine development.
Read more about this topic in detail
What the UK did right

The UK government can be praised for its very early handling of the pandemic in January and February 2020. On the 31st January 2020, the first two cases of COVID-19 were identified in England. They were quickly transported to a regional infectious diseases unit. The UK also required individuals who had flu-like symptoms returning from China, Hong Kong, Malaysia, Korea, Singapore, Taiwan, and Thailand to self-isolate for 14 days. The UK adopted contact tracing: a fundamental part of outbreak control that is used around the world to prevent the spread of infections. This was effective at preventing the early spread of COVID-19 throughout the UK.
The UK government invited thousands of doctors, nurses, midwives and other healthcare professionals who had recently retired to return to work. Over five thousand medical students were also brought into the workforce. This required medical schools to move final year medical students’ graduation forward. These measures helped the NHS to meet the increased staffing demand created by COVID-19. To provide extra critical care capacity the UK government built temporary hospitals across the UK. The first hospital to open was the NHS Nightingale Hospital London which opened on the 3rd April. Since then, seven NHS Nightingale hospitals have been built. In addition the NHS managed to free up 33,000 additional beds across the UK. They achieved this by cancelling non-urgent treatments as well as working with the private sector to increase capacity. To accomplish this in a relatively short space of time was an impressive achievement.
With regards to financial support one of the biggest measures taken by the UK government was the Coronavirus Job Retention Scheme. This was introduced to help employers who could not afford to maintain their workforce as their business was affected by COVID-19. This was also known as ‘furlough’, a scheme in which the government pays up to 80% of a furloughed employee’s wages. At the scheme's peak in May 2020, 30% of the workforce across the UK was furloughed. The UK government also implemented economic stimulus measures to help companies and the economy as a whole. This included interest-free loans schemes for small businesses as well as loans for large businesses. The UK government also provided £750 million of funding for frontline charities across the UK, including hospices and those supporting domestic abuse victims.
The UK government has invested millions of pounds into research for COVID-19 vaccines and potential treatments. The University of Oxford conducted the RECOVERY trial which discovered the first treatment shown to reduce mortality in COVID 19 patients: Dexamethasone. This was an extraordinary achievement and demonstrated the collective strength of the NHS. On the 17th April 2020 the UK government announced the formation of a new government led ‘Vaccine Taskforce’ aimed to support the rapid development of a coronavirus vaccine by providing industry and research institutions with the resources and support needed. As of January 2021, two vaccines have been approved in the UK. The first was the Pfizer/BioNTech vaccine and the second was the Oxford-Astrazeneca vaccine.
On top of this, the UK has given £500 million to a new global vaccine-sharing scheme designed to ensure that treatments for COVID-19 are distributed fairly around the world. The Prime Minister, Boris Johnson, also promised £340 million to the World Health Organisation over the next four years. This is a 30% increase on previous years and shows that the UK government is committed to global public health.
Read more about this topic in detail
What the UK could have done better

Research from The Health Foundation showed that support for the government’s handling of the pandemic has decreased over time. In May 2020, 60% of the public thought that the government was handling the pandemic “well”. This reduced to only 43% by July 2020.
A criticism of the UK’s COVID-19 response is that they acted too slowly to initiate measures such as the first national lockdown. The number of positive cases began to rise rapidly from the 1st March, however a lockdown was not implemented until the 23rd March. Countries such as Spain, Italy and France initiated lockdown measures earlier. The British Medical Journal was particularly critical of the UK government saying that it did “too little, too late”. They argue that the World Health Organisation declared an emergency on the 30th January, so why did the UK wait until the 23rd March to impose a lockdown?
The second criticism of the UK’s COVID-19 early response is that they under-delivered on their promises for COVID-19 testing as well as in contact tracing. The UK government decided to abandon its contact tracing strategy on the 12th March 2020. The UK government moved testing capacity only to patients admitted to hospital. This drew negative feedback from some public health experts.
Resource allocation is another domain that was negatively viewed. Millions of pounds were invested to construct the Nightingale hospitals, however as of May 2020, only 51 patients were treated at the 4000 bed NHS Nightingale Hospital in London. A research report from the Institute for Social and Economic Research concluded that almost two-thirds of patients in the UK with common life-threatening conditions have been denied care by the NHS because hospitals were focused on fighting COVID-19.
The COVID-19 pandemic caused an extraordinary impact on the global demand and supply of PPE. The UK government has been criticised for failing to stockpile adequate protective equipment to cope with a pandemic. There were no gowns, visors, swabs or body bags in the government’s pandemic stockpile when COVID-19 reached the UK.
The final critique of the UK’s COVID-19 response was of the government’s mixed messages in communication. This was particularly seen over the Christmas period in the UK. Some people have said that the government gave out confusing Christmas coronavirus rules. It is a challenge for any government to communicate effectively with the public; this is particularly true in a pandemic situation as the information is constantly changing and can be quite technical in nature.
Read more about this topic in detail
The Impact of COVID-19 on Patients

General impact on patients
The COVID-19 pandemic has had a huge impact on the core, day-to-day, services offered by the National Health Service. The NHS had to make difficult decisions to ensure that they freed up enough capacity to deal with the new wave of patients that they expected to enter hospital with COVID-19.
In addition to the reduction in services by the NHS, fewer patients were willing to seek care during lockdown for fear of catching COVID-19. The combination of reduced NHS services and patients being scared to seek help has meant that millions of patients missed appointments.
More than 2.2 million people deemed as ‘clinically extremely vulnerable’ were advised by the government to shield during the COVID-19 pandemic. This meant they could not leave their homes until the end of May 2020. A survey by the Office of National Statistics found that 35% of people shielding said that their mental health worsened and that 20% said that they were unable to access certain types of care, such as tests and scans.
Read more about the impact on patients in detail
Patients with chronic diseases
Some of the most impacted chronic conditions during the COVID-19 pandemic are diabetes, chronic obstructive pulmonary disease (COPD), and high blood pressure (also known as hypertension).
Diabetes

People with diabetes are at an increased risk of serious illness from COVID-19. A study from NHS England revealed that one in three people who have died in hospital in England following a diagnosis of COVID-19 also had diabetes.
People with diabetes usually have regular check ups to keep them as healthy as possible. Diabetes care has changed during the pandemic with a shift to online appointments where possible. There has been a push to encourage people with diabetes to closely monitor factors like their blood sugar and feet themselves.
Chronic Obstructive Pulmonary Disease (COPD)
Chronic obstructive pulmonary disease (COPD) is a condition that makes it difficult to empty air out of the lungs because the airways have become narrowed. The usual treatment for COPD involves inhalers and pulmonary rehabilitation. In a study, published in The Lancet medical journal, it was shown that patients with severe COPD had a higher risk of death from COVID-19 than patients without COPD. Another study looked at the impact of COVID-19 on people living with COPD in the UK. The study found that patients with COPD were living with increased levels of anxiety, reductions in their physical activity and reductions in the number of visitors during periods of lockdown.
Hypertension

Having high blood pressure alone does not place a patient in the ‘shielding’ category for extremely vulnerable clinical patients. However studies show that poor blood pressure control is independently associated with an increased risk of death from COVID-19. It is estimated that, in England alone, there are more than five million people who suffer from undiagnosed high blood pressure. As high blood pressure typically presents with no symptoms, it is often only picked up by screening or when patients present to their doctor for something completely unrelated. As less people visit their doctor and as face-to-face consultations are reduced, there is a real risk that more patients will continue living with undiagnosed high blood pressure and the risks associated with it.
Read more about the impact on patients in detail
Cancer patients
The British Medical Association estimates that in England between April to June 2020, there were between 274,000 and 286,000 fewer urgent cancer referrals. It also estimates that there were between 20,800 and 25,900 fewer patients starting first cancer treatments following a decision to treat. The diagnosis and treatment of cancers can be highly time-dependent and delays in treatment could have serious harmful consequences for patients.
Patients with cancer are also at an increased risk from COVID-19. This is because cancer and its treatment can weaken the immune system and the ability to fight infection. During the pandemic, doctors have had to weigh up the benefits of chemotherapy with the risk of bringing cancer patients into hospital with the risk that they may catch COVID-19. With shielding advised for many cancer patients another issue has been their inability to receive support from friends, family and specialist groups.
Read more about the impact on patients in detail
Patients over 60 & Care Homes

There is substantial evidence that the older you are, the more likely you are to die from COVID-19. Research data from May 2020 revealed that 4 in 5 people who had died from COVID-19 were aged 70 or over. Analysis of critical care data showed that approximately 2 in every 5 patients who receive critical care for COVID-19 did not survive. For patients aged 50 or less, 1 out of every 5 patients died. For patients aged 70 and over, 3 out of every 5 patients died.
Care homes have been badly hit by COVID-19. People in care homes are typically in their 80s and 90s and are also often living with underlying health conditions; this makes them especially vulnerable to serious consequences if they catch COVID-19. Another factor to consider is that staff often have to provide personal care to residents, requiring them to come into close contact with many residents and risking the spread of the virus.
Age is an important consideration in assessing risk from COVID-19, but remember that age is not the only factor that should be considered. Gender, ethnicity and pre-existing medical conditions are also known to increase risk from COVID-19.
Read more about the impact on patients in detail
Patients in BAME communities

A report from Public Health England found that the risk of dying from COVID-19 in the UK is higher if you are from a Black, Asian and Minority Ethnic group. In this analysis, people of Bangladeshi ethnicity were found to have twice the risk of death than people of White British ethnicity. People of Chinese, Indian, Pakistani, Other Asian, Black Caribbean and Other Black ethnicity had between a 10% and 50% higher risk of death from COVID-19 compared to White British. It was found that many of the pre-existing conditions that increase the risk of having a more severe infection, such as having diabetes, were more common in people from BAME groups. Public Health England found a strong link between economic disadvantage and COVID-19 diagnoses and severe disease. BAME groups tend to have poorer socioeconomic circumstances which lead to poorer health. It has been suggested that COVID-19 did not create health inequalities, but rather the pandemic exposed long standing health inequalities affecting BAME groups in the UK.
Read more about the impact on patients in detail
Conclusion
A question on COVID-19 is very likely to come up in medical school interviews this year. With use of reliable resources it is essential that you are upto date with the latest developments and can clearly discuss the impact of COVID-19 on patients, the public and on healthcare professionals.
Questions about COVID-19 could arise in many formats such as ethical dilemmas, being asked your opinion on an aspect of how the pandemic has been handled or even what you have learnt from the pandemic. Try to think of some questions and practice your answers; making sure they are informed and well-balanced. We understand that this is a vast subject but hope that this article has given you a helpful overview of the main topics to consider.



